Anthony Yi, MD
Orthopedic Surgeon
Foot and Ankle Specialist
Seattle, WA
I am excited and honored to announce that one of my studies (titled “The Lateral Drawer Test: A New Clinical Test to Access Mortise Instability in Weber B Fibula Fractures”) was published in Foot & Ankle Orthopaedics (the official journal of the American Orthopaedic Foot & Ankle Society)!
I am particularly grateful for the opportunity to have worked with such wonderful people. My co-authors who conducted this study are people I hold in the highest regard.
I am also honored to have participated on a team of brilliant minds from all around the globe! I thank my co-authors (who did most of the legwork)!
I believe that this study is emblematic of one of the invaluable lessons that I learned during my time at Harvard – never settle and always strive to improve patient care. I was always impressed by my mentors who, despite being leaders in our field, constantly asked of themselves how they could be better.
With regards to the study itself:
As orthopedic surgeons, one of the most difficult decisions can be answering if we should treat a particular injury with or without surgery.
When it comes to an ankle fracture (AKA broken ankle), the decision hinges upon whether the fracture is stable or unstable.
A stable ankle fracture is one in which the ankle joint remains reduced (everything lines up and is in the correct position despite there being a fracture or broken ankle). These can be treated without surgery.
An unstable fracture is one in which the ankle joint does not remain reduced under normal load (there can be an obvious or subtle change in the ankle joint, which does not line up perfectly). These should generally be treated with surgery (however, a patient’s situation is sometimes complicated and surgery may not be the best pathway).
Determining if an ankle fracture is stable (can be treated without surgery) or unstable (most likely needs surgery) is not always straightforward. In fact, it is often very difficult and fractures rarely “follow the textbook.”
There are several methods of testing the ankle to determine if it is stable or unstable. The most common way is to perform a “stress test,” which involves putting stress through the ankle while taking an x-ray to see if there is any change compared to an x-ray without stress.
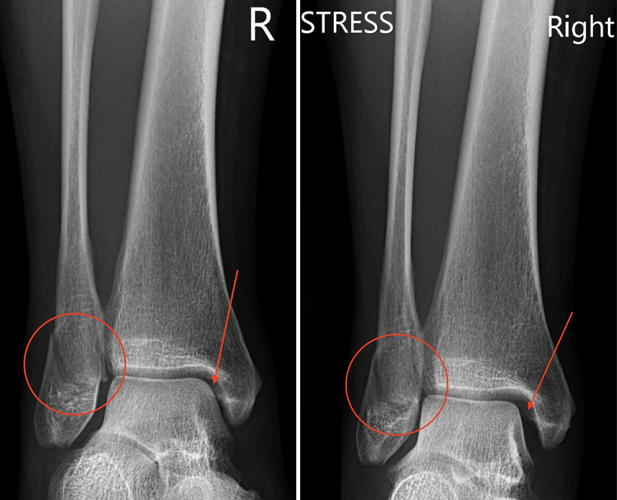
Here is an example of a stress test. On the left is an x-ray of a right ankle fracture. The red circle shows the fracture. On right is an x-ray of the same ankle, but with stress applied (ankle is rotated outwards while taking the x-ray). Notice how much bigger the black space (red arrow) is on the stress x-ray on the right side compared to the regular x-ray on the left side! This change in the ankle joint shows that there is instability.
In this study, we looked into trying a simple physical exam test (without x-ray) to see if we could detect instability in fracture/broken ankles.
This test involves holding the tibia (shin bone) stable with one hand and grabbing heel and shifting the ankle out (away from the big toe side). We named this the “lateral drawer” test.
In summary, we found that the lateral drawer test was very good at detecting ankle fracture (fibula fracture) instability.
- Sensitivity of 83%: using the test, we could determine 83% of the unstable ankle fractures
- Specificity of 97%: using the test, we were correct 97% of the time we thought the ankle was stable
- Of note, these percentages were calculated by comparing to what we consider the ideal “gold standard” way of detecting ankle instability (the ankle stress test under x-ray).
Also, patients did not experience significant pain while the lateral drawer test was performed on their ankle.
Ultimately, while the test is not perfect (we still missed 17% of unstable fractures while using it), it can be very useful in that it provides an extra good data point that can help us to determine if an ankle fracture is unstable or stable – especially given that interpreting the tests/tools (that we use for determining if an ankle fracture is unstable) are not always crystal clear. There is certainly a large “gray” area when it comes to determining if someone needs to have their ankle fracture fixed.
Part of the fun of being an orthopedic surgeon is constantly striving to improve – which involves determining which questions are important and finding clever ways to answer those questions.